At least one in every four people living with a terminal diagnosis will experience depression, anxiety, adjustment disorder or low mood.
Many more will experience distress because of deteriorating health and related uncertainty. Feelings of hopelessness, discouragement and even a desire for hastened death can occur.
People have reported that psychological support helps them develop better coping strategies, helps them be more open to their situation and improves communication with their families and those involved in their care.
An advanced or life-threatening illness brings with it significant additional physical, psychological, social and spiritual concerns.
Many people living with a terminal illness adapt and cope with support from those close to them. For some people, additional support from a counsellor or trained professional is needed, though access to such support is not routinely available to everyone who might benefit.
Physical symptoms are more easily recognised and described, so tend to be prioritised over psychological symptoms. But mental wellbeing is as important as physical wellbeing, and both are interconnected.
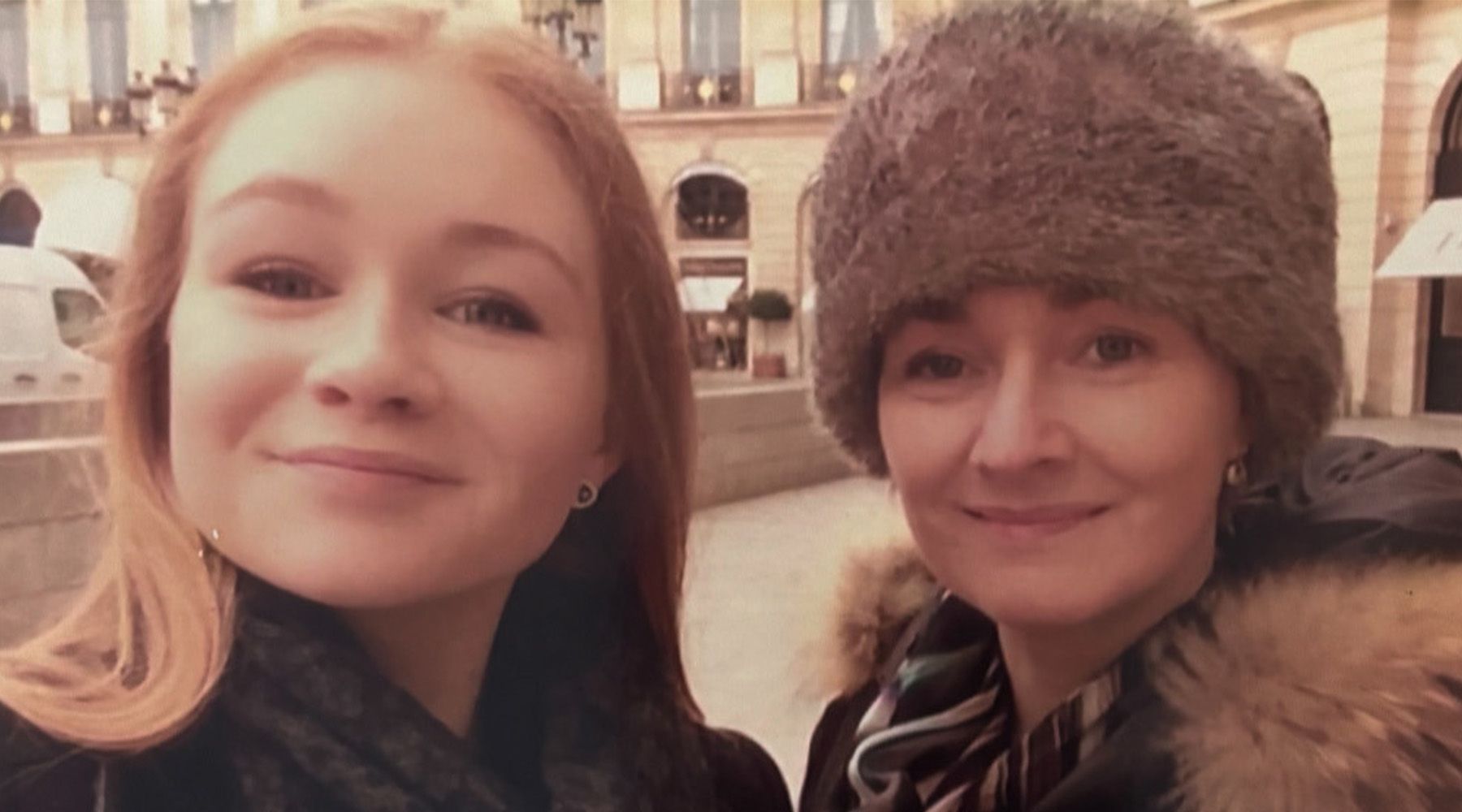
Family members also need mental wellbeing support. One person talked to us about the challenges of coping with a terminal illness when you have children. They found that their illness had a major impact on their child's emotional wellbeing, impacting social and school behaviour, which caused them more stress, worry and anxiety.
Different therapeutic approaches
There is a wide range of therapeutic approaches that have value to people impacted by terminal illness, yet access is often limited due to a shortage of trained professionals to deliver such interventions or funding to resource them.
For example, Cognitive Behavioural Therapy (CBT) can help people develop adaptive coping skills, Acceptance and Commitment Therapy (ACT) can help people become more open and aware of their situation, and to connect with their values and what is most important to them. Mindfulness can help people manage overwhelming negative emotion and focus on the present moment, and dignity therapy supports people to connect with a sense of meaning and purpose.
These different therapeutic approaches each have a slightly different focus, though all aim to improve the mental wellbeing of the person living with a terminal illness.
More support is needed
Right now, there isn't enough specialist mental health support available for people living with a terminal illness, and those close to them – meaning people are experiencing unnecessary distress at the end of their lives.
Palliative care professionals are often experienced in providing holistic care that addresses psychological, social and spiritual needs. However, we need to upskill all healthcare professionals in the principles of evidence-based psychological therapies such as CBT, ACT and mindfulness.
Online mental health and wellbeing resources, that can be accessed by anyone at any time, are essential. It would also be useful to harness digital technology, so that people can track their wellbeing, or access support if they have concerns.
We need to be routinely assessing people's mental health needs so they can be signposted to appropriate psychological support if needed.
For people with pre-existing mental health conditions, and those facing complex challenges associated with their terminal illness, access to a clinical psychologist can be helpful. Clinical psychologists and mental health specialists also have an important role to play in training, mentoring and upskilling other professionals.
A space to learn and share
In January 2024, we launched a Mental Health and Wellbeing in Advanced Illness Network (MAIN), funded by Marie Curie, which so far has over 350 members, including health and social care professionals such as psychologists, researchers, policy people, service managers and social workers, and members of the public.
MAIN runs webinars and events to support research and knowledge exchange in relation to improving mental health and wellbeing for people with a serious life-limiting illness.
One of our recent webinars was focused on identifying psychological distress in palliative and end of life care.
Visit the Mental Health and Wellbeing in Advanced Illness Network (MAIN) website.